Abstract
Introduction: Gemtuzumab ozogamicin (GO; MylotargTM) is an antibody-drug conjugate composed of an anti-CD33 monoclonal antibody covalently linked to the potent antibiotic calicheamicin. Previous studies have shown GO is generally well tolerated and can induce durable second remissions when administered as monotherapy or in combination with chemotherapy in patients with relapsed or refractory (R/R) acute myeloid leukemia (AML). We report safety data from an expanded-access protocol (EAP) that allowed compassionate use of GO in patients with R/R AML or acute promyelocytic leukemia (APL) and no access to comparable or alternative therapy.
Methods: Conducted in the United States, the GO EAP (NCT02312037) was an open-label study in patients aged ≥3 months with R/R AML (including myelodysplastic syndrome) or APL who were considered to have the potential to derive clinical benefit and had exhausted other treatment options. The protocol allowed for treatment regimens tested in clinical trial settings and reported in the Mylotarg Investigators Brochure or peer-reviewed journals. Data from these trials indicated these regimens could potentially benefit a patient with R/R AML or APL. For R/R AML patients, the regimens included GO as monotherapy or in combination with anthracyclines and/or nucleoside-analogue containing regimens or hypomethylating agents. For patients with APL, these included GO as monotherapy or in combination with all-trans retinoic acid and/or arsenic trioxide. Patients were permitted to re-enroll in treatment, and their data are summarized according to each enrollment treatment.
Results: A total of 331 patients received GO either as monotherapy for R/R AML (adult [aged ≥18 years]: n=118; pediatric [aged <18 years]: n=21), combination therapy for R/R AML (adult: n=99; pediatric: n=84), or treatment for APL (adult: n=9; pediatric: n=0). Mean age in the monotherapy, combination therapy, and APL groups was 55, 32, and 57 years, respectively.
The most frequently administered doses of GO in the monotherapy group were 9 mg/m2 (1 dose: n=21 [15%]; doses on ≥2 days: n=29 [21%]) and 3 mg/m2 (1 dose: n=10 [7%]; doses on ≥2 days: n=33 [24%]). Nearly all patients in the combination-therapy group received 3 mg/m2 (1 dose: n=96 [53%]; doses on ≥2 days: n=76 [42%]). GO 6 mg/m2 was the most frequently administered dose in the APL group (1 dose: n=3 [33%]; doses on ≥2 days: n=4 [44%]). Treatment was discontinued in 94 (68%), 71 (39%), and 3 (33%) patients in the monotherapy, combination-therapy, and APL groups, respectively. Common reasons for discontinuation included resistant disease (monotherapy: n=25 [18%]; combination therapy: n=16 [9%]; APL: n=1 [11%]), adverse events (AEs) not related to study drug (monotherapy: n=7 [5%]; combination therapy: n=3 [2%]; APL: n=1 [11%]), and AEs related to study drug (monotherapy: n=6 [4]%; combination therapy: n=4 [2%]; APL: n=0).
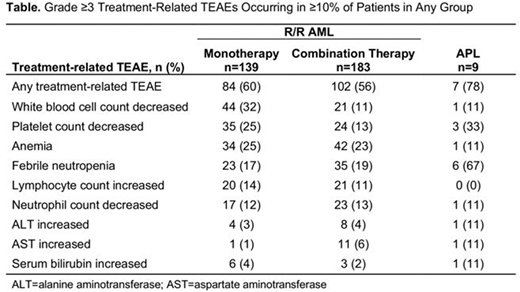
All-causality grade 5 AEs were reported in 114 (34%) patients: 72 (52%), 40 (22%), and 2 (22%) in the monotherapy, combination-therapy, and APL groups, respectively. The most common grade 5 AEs (excluding disease progression and AML) were sepsis in the monotherapy group (n=7 [5%]; 4 treatment-related), respiratory failure in the combination-therapy group (n=5 [3%]; 1 treatment-related), and intracranial hemorrhage in the APL group (n=1 [11%], not treatment-related). Grade ≥3 treatment-related, treatment-emergent AEs (TEAEs) were reported for 84 (60%) patients in the monotherapy group, 102 (56%) patients in the combination-therapy group, and 7 (78%) patients in the APL group; hematologic TEAEs were most common, followed by hepatic TEAEs (Table). Possible hepatotoxicity was reported in 5 patients: 1 case each of veno-occlusive disease (VOD) and drug-induced liver injury in the monotherapy group and 2 cases of veno-occlusive liver disease (1 fatal) and 1 case of VOD in the combination-therapy group.
Conclusions: GO was generally well tolerated; only a small proportion (<5%) of patients in each group discontinued treatment due to treatment-related TEAEs. The most frequent treatment-related, grade ≥3 TEAEs were hematologic. The incidence of hepatotoxicity was low across all cohorts. The results suggest GO is an important treatment option for patients with R/R AML or APL.
Wang:Jazz: Speakers Bureau; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy; Amgen: Consultancy; Jazz: Speakers Bureau; Novartis: Speakers Bureau; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Speakers Bureau; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees. Chirnomas:Pfizer Inc: Employment, Equity Ownership. Fazal:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Jazz: Membership on an entity's Board of Directors or advisory committees; Pfizer: Speakers Bureau. Lin:Jazz Pharmaceuticals: Honoraria. Nand:Pfizer: Honoraria. Pierce:Pfizer Inc: Employment, Equity Ownership. Shami:JSK Therapeutics: Employment, Equity Ownership, Membership on an entity's Board of Directors or advisory committees; Lone Star Biotherapies: Equity Ownership; Baston Biologics Company: Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy. Vermette:Pfizer: Employment, Equity Ownership. Abboud:Agios: Honoraria; Jazz: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal